By M.J Ellington

Photo by Julie Bennett
Looking at a year of unbelievable pandemic, health care providers in rural Alabama say the crisis shows how vital rural hospitals and their medical communities are to the health of rural Alabama.
Three health providers tell how Alabama provides care in complicated times, including one nurse who worked in a hospital COVID-19 unit until she got the virus.
A race to save a life
When Selma resident Safiya Johnson thinks about COVID-19, she can look in the mirror and find someone hit by the pandemic. A registered nurse, Johnson worked at a busy Montgomery hospital COVID unit from March 2020 until she became ill in late August.
“Because I had worked around it and with it as a nurse, it was no surprise,” she says. When the mild symptoms she had for a few days worsened and Tylenol would not bring her fever down, she headed to the hospital in Selma. A couple of days later, she was on a ventilator, in a medically induced coma and headed to University Hospital at UAB in a special COVID ambulance staffed with a doctor and nurse.
Johnson has little memory of her weeks at UAB, but she has constant reminders that COVID-19 can leave debilitating symptoms long after the virus leaves the body.
Some of her aftereffects, termed post-COVID or long-COVID syndrome, include difficulty walking and diminished feeling in hands and feet. Johnson still requires some help dressing, eating and doing other tasks most people take for granted. But she no longer walks with a walker and is beginning to drive short distances again near her home.
Johnson said while she was in intensive care at UAB, she stopped urinating and was put on dialysis. “They never expected me to come off of dialysis; they told me that,” she says. Then in late January, she started urinating again. By testing her urine analysis and potassium levels, her doctors determined that she no longer needs dialysis. Johnson’s mother, Marilyn Simpson, helps with daily living tasks, including driving her to appointments.
Johnson wonders what would have happened if the hospital in Selma had not had a connection to UAB that helped her transfer to a special COVID treatment facility rapidly. She wonders what happens to people in rural Alabama who don’t have a nearby hospital, health insurance, access to specialized care or transportation. She is grateful that Baptist Medical Center East, where she worked in Montgomery, still pays for her health insurance coverage and that the company provides occupational and physical therapy.
She plans more schooling for a degree as a nurse practitioner.

Community deserves honest communication
In Chatom, Washington County Hospital and Nursing Home CEO Teresa Grimes said the pandemic hit her town of 1,200 hard, affecting the hospital and adjacent nursing home in spring of 2000. Grimes said the response of people in her town and county meant a lot.
“COVID proved that rural hospitals and healthcare providers are vital, critical infrastructure,” Grimes says.
The hospital shut down “anything that was elective,” to focus on patients and staff dealing with COVID, Grimes says. During the worst weeks, area churches organized nightly prayer walks and brought snacks for healthcare workers. Dr. Steve Donald, the facility’s medical director, temporarily shut down his private medical practice to focus on hospital and nursing home patients and staff, she says.
“As painful as it was, we were honest about what was going on,” she says. The facility did daily updates on Facebook detailing how many residents and employees had the virus, as well as when someone died.
Federal funds helped fill gaps
Federal COVID relief funds have not made the facility wealthy, but Grimes said they helped make up revenue lost when elective medical procedures and services temporarily stopped. She hopes people in rural areas will take advantage of the services and convenience of their local hospitals. “We depend on the volume of service and appreciate and need for people to use our services,” Grimes says.
COVID funds paid for things that Grimes said would be unaffordable otherwise. They include hazardous duty pay for employees during the worst pandemic weeks, a portable x-ray machine, and negative pressure machines to direct air flow that helps control the virus. The facility also used COVID funds for testing sites and now conducts multiple drive through COVID vaccination clinics around the county.
“It has been a tough year for everybody, but we have put our all into caring for each other and our communities,” Grimes says.
Physician’s heart in rural health care
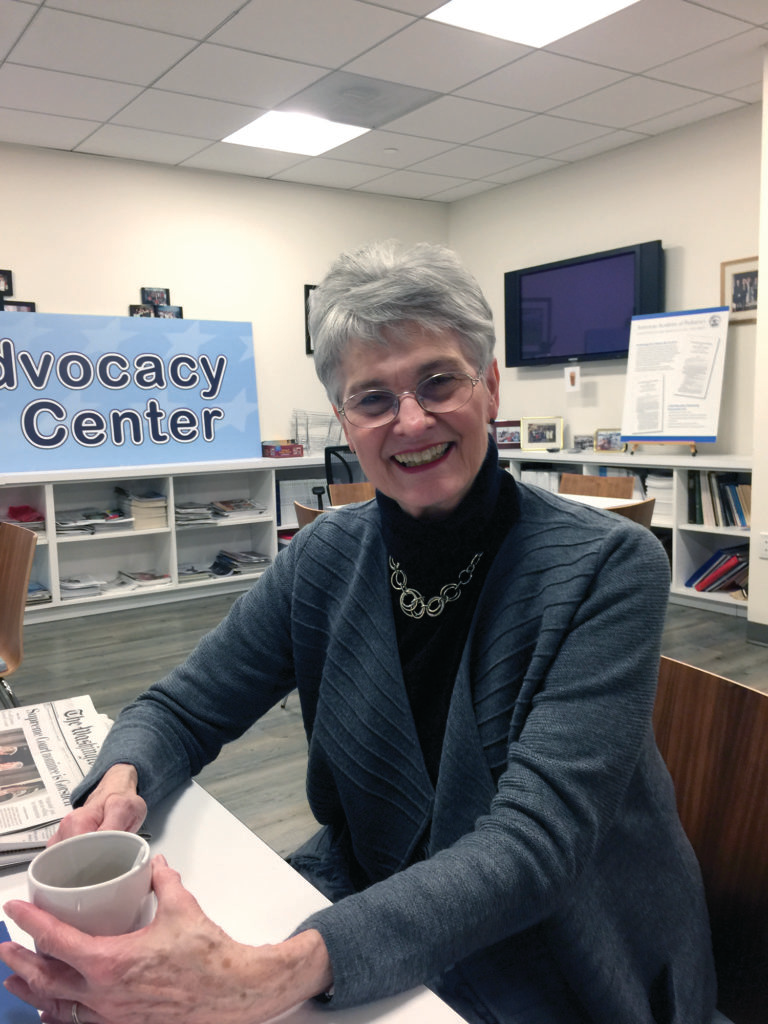
In Brewton in Escambia County, Dr. Marsha Raulerson, a semi-retired pediatrician, divides her time between treating 100 special needs children and volunteer advocacy for better health policy for children and Alabamians living in poverty.
A proponent of telemedicine and increased broadband technology to connect rural doctors and patients to services elsewhere, Raulerson began offering telemedicine options for her patients and their families. Her newest program is part of Pediatric Access to Telemental Health Services, or PATHS. The Department of Mental Health – Children’s of Alabama grant program increases the capacity of primary care providers in rural Alabama to diagnose, treat and manage mental health conditions in children and teens.
Raulerson came to Brewton with her husband, a nephrologist recruited to fill a south Alabama physician gap in care for kidney diseases and related conditions.
She thought the couple might stay a few years. The quality of life drew the family in spite of the fact that a critical federal formula means physicians in small towns get paid less than doctors near large medical centers. Alabama has the lowest federal reimbursement rates for services to Medicare patients in the country and physician pay is tied to the reimbursement rate, she says.
Raulerson says over 40 years, she’s seen young doctors come to the small city for a few years then leave for a practice linked to a larger medical center for better pay. Nurses also leave for the same reason. The physician drain in rural communities is concerning, she says, but if the federal reimbursement rate is not changed, perhaps a lower tax rate for doctors there could be considered, she says.
“People like me, we have the same training but the pay is different because we are in a small town,” she says. “I have been extremely lucky because my husband is a medical inventor and he had a number of patents.” The patents gave the couple the financial means to live comfortably with small town doctor income and send three children through college.
While people may wonder if the federal COVID and economic recovery relief funds would help rural hospitals and providers, Raulerson says when the federal government ordered hospitals and care providers to stop all routine services and procedures to slow the pandemic in spring 2020, the financial hit affected them all. The COVID funds just help fill the financial hit of that period.
Raulerson is an advocate of Medicaid expansion in Alabama to help people in rural communities be healthier with access to regular care and boost the local economies. But she believes the COVID experience had some positive impact. “Our hospitals will be better prepared for any future pandemic,” she says.
Challenges in Alabama’s rural areas
Even before the COVID-19 pandemic virus shut down life as usual around the world, Alabama’s rural health care system faced constant hurdles. Figures from the Alabama Hospital Association explain how.
The rural population tends to be older and fewer people have health insurance to pay for care. They often delay care and then use the hospital emergency department for care because there’s no other choice.
Alabama is one of only 12 states that did not expand Medicaid, the federal health coverage for the lowest income people. Without health coverage, there may be no way to pay the bill, leaving hospitals with debt for the care.
A federal formula that determines Medicare payments for hospitals and health providers sets lower reimbursement rates for rural hospitals and health providers than in larger cities.
The result is that 87% of rural hospitals operate in the red.
Two federal changes during the pandemic show possibilities that Alabama could make to reverse the downward trend for rural health care funding. The American Rescue Plan Act will increase Alabama funding by $940 million over two years and could be used to expand Medicaid; and the Families First Coronavirus Response Act temporarily increased the federal reimbursement rate for health care providers.